
Diabetes burnout
A build-up of diabetes distress can tip into periods of “diabetes burnout” where a person with diabetes might start to avoid self-management tasks for more significant periods of time; this then has the potential to impact upon their physical health.

People with diabetes burnout often recognise the importance of caring for their diabetes, but feel unable to make any changes.
Diabetes burnout is different to depression. Whilst depression (click here for more information) causes a person to have negative thoughts about themselves, others, and a sense of hopelessness about the future, diabetes burnout is associated with thoughts and feelings specifically about diabetes. The individual may not seem particularly low in mood to the outside world. It can happen at any age although the longer you have had diabetes, the more prone you are to feeling burnt out.
Thoughts
- My diabetes is out of control
- I can’t be bothered
- My diabetes controls everything
- No one understands what it is like to live with diabetes
- I am alone
- Nothing will work to improve my diabetes
Feelings

- Angry
- Overwhelmed
- Defeated
- Frustrated
- Worried
- Sad
- Helpless
- Unmotivated
Behaviours
- Avoiding diabetes-related tasks like glucose monitoring and carb counting
- Avoiding healthcare appointments
- Stopping giving insulin
- Doing nothing
- Unhealthy eating
- Risk-taking behaviours
Click on the items below for more information:
No Result
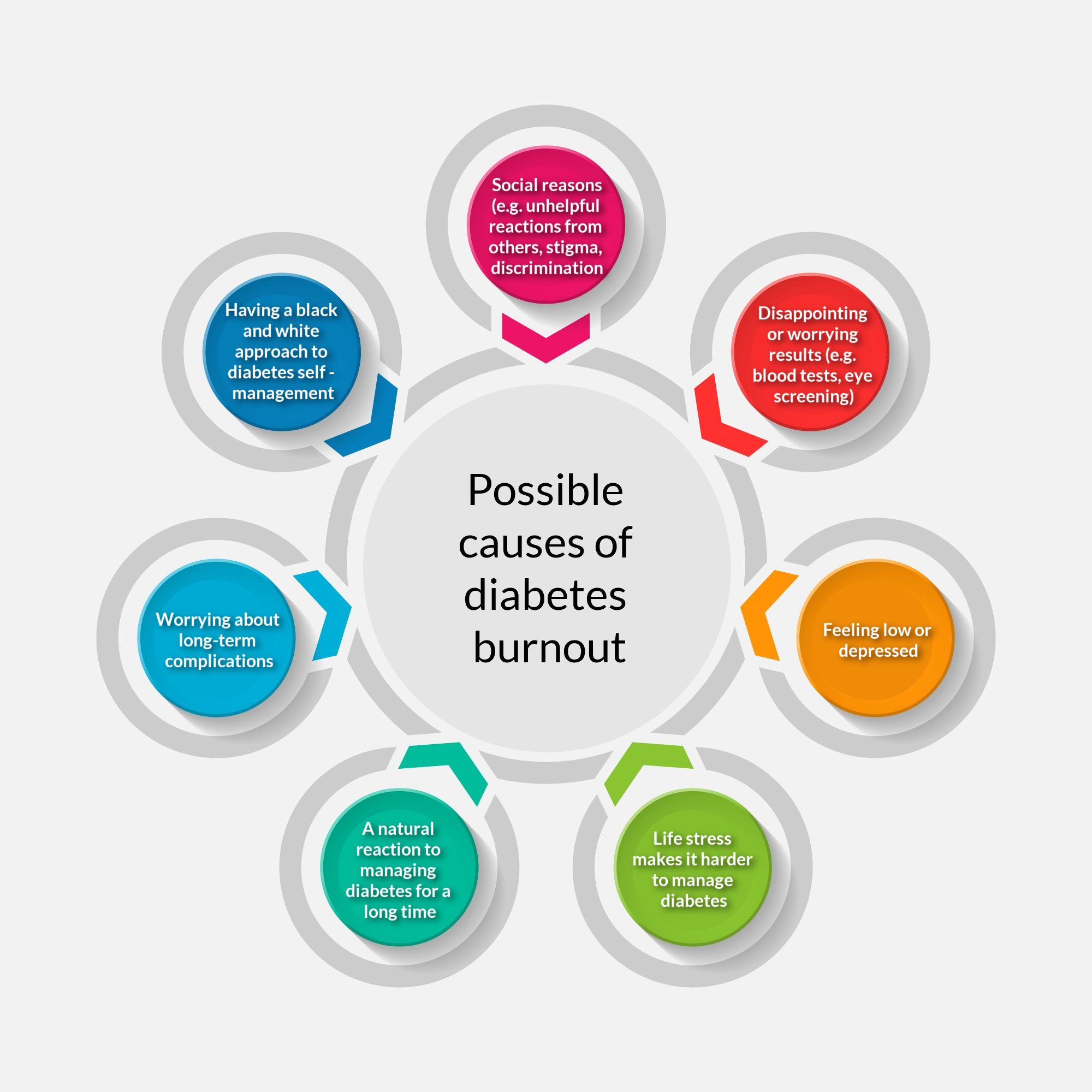
Diabetes burnout has many different causes and triggers, and people may identify several reasons that have built up over time (think back to the stress bucket). Here are some examples:
- reduction or stopping of usual diabetes management (e.g., missing healthcare appointments, avoid checking glucose levels, less healthy eating)
- higher glucose levels leading to increasing HbA1C
- more frequent and severe hypoglycaemia
- feeling ashamed, angry, low in mood, or anxious
- difficulties within personal relationships (e.g., with family and friends)
- impaired quality of life
- it is a relatively new concept, and they may not be aware of it
- diabetes is often managed medically, and conversations might focus on blood test results, not emotions related to diabetes
- some healthcare professionals might feel they do not have the right skills to support people if they open up a conversation about emotions and diabetes
- appointments are time-limited, and you may both avoid talking about what it means to live with diabetes if it seems there is not enough time
Hover over this image of Faizah to see her advice on diabetes burnout.

Naomi
Is there anything I could do to help myself?
Support from an appropriately trained healthcare professional can be really helpful for people with diabetes distress or burnout. But there are many self-help actions you can take, both to overcome and also reduce your likelihood of experiencing burnout. Click on the items below to find some ideas, with links to worksheets that you might find helpful:
-
- Know how your thoughts, feelings, and behaviours interlink and affect each other Identifying cycles of thoughts, feelings & behaviours worksheet
- Know your personal warning signs of burnout (e.g., missing short-acting insulin a few times a week, missing clinic appointments, guessing carb content rather than accurately calculating, reducing blood glucose monitoring) Personal warning signs worksheet
- Give yourself permission to feel "negative" emotions like frustration and anger towards diabetes – they are a healthy response to its demands.
- Recognise that pushing difficult thoughts and feelings away can be very tiring and they often pop back up, despite our efforts. It’s a bit like trying to push a beach ball under the water for a long period of time. Like difficult thoughts and feelings, it can be more helpful in the long run to let the ball float alongside you.
- It can be helpful to try and name the thoughts and feelings you are experiencing, and work to accept they are a normal part of living with a long-term condition like diabetes (for example: “I am having the thought that I hate diabetes” or “I am feeling angry about diabetes”).
- Try practicing some relaxed breathing, or mindfulness exercises – there are lots of great videos on YouTube or mobile phone apps which guide you through some mindfulness practices. Relax Breathing Worksheet
Faizah
- Catch unhelpful ways of thinking about diabetes self-management such as perfectionist thinking or ‘black and white thinking’ – try to think of the bits in between – things are rarely all good or all bad. Black and white thinking worksheet

Faizah
- Accumulation of stress can make it harder to cope with the demands of life with diabetes.
- It can be helpful to think about your own ‘stress bucket’ – notice what fills up your bucket, and think of ways to let some of the water out. Stress bucket worksheet
- Aim for small, realistic goals and build up
- Diabetes is a long-term health condition so pace yourself to cope over time by not being too perfectionistic
- Be flexible - Having separate diabetes management plans for difficult days and easier days can be helpful.
- On easier days you might find you have the time and energy to fully carb count your meals, give your insulin before you eat for most meals and check your glucose levels regularly, aiming to be in range for a larger part of the day.
- On more difficult days you might find it easier to eat foods you already know the carb content for, you might check in on your glucose levels less often and plan to give your insulin with food or after. Find goals that work for you. Setting goals worksheet
- Talk to someone involved in your diabetes care about the way you are feeling about your diabetes
- Talking about your experiences of diabetes to others who understand, can also help. Contact Diabetes UK support groups or visit blogs such as those on www.diabetes.org.uk.
- See our list of places to go for help and support below.
- Look after yourself when you are going through a stressful life event. Diabetes management may need to be given less priority for a time until life has returned to "normal". Consider the minimum you need to do to care for your health. You may want to make easier and difficult day goals (see goal planner worksheet).
- Be kind to yourself - remember there are over 40 things that can affect your blood glucose levels every day and you won't get it right all the time.
- Ask yourself, what would I say to a close friend who was facing similar difficulties?
- Think of one diabetes self-care task you are avoiding that you could do today, and congratulate or reward yourself for doing it.
- Who in your life has been the person to get the best out of you? Maybe someone from your current day to day life or someone from your past - maybe a favourite teacher, supportive coach or maybe a grandparent or aunt / uncle? What was / is it about this person that got the best out of you? What qualities did they have and how did they speak to you?Maybe they were encouraging, or held hope for you, maybe they were balanced or fair in their opinions of your efforts or maybe they were good at seeing the bigger picture?Could you aim to try to take this same approach when talking with yourself about your diabetes management? After all, if it has worked in the past maybe this would be a helpful approach!
Faizah
- It can be helpful to think of the pros and cons of taking steps to managing your diabetes more effectively. Listing the reasons you have for wanting to manage your diabetes can help remind you why it is important and can motivate you to take the first steps.My reasons for diabetes self-care worksheet
Person with type 1 diabetes
You can use two two worksheets to help you gain more understanding of diabetes burnout:
Where can I get support if I am worried about diabetes distress or burnout?
 | Diabetes UK is a national charity that supports individuals with diabetes and their families or carers. It can be contacted online, over the phone, or by post (https://diabetes.org.uk / 0345 123 2399). |
 | Some diabetes teams have a psychologist who may be able to offer support – ask your team if this service is available where you live |
 | Talk to another healthcare professional who you trust, like your GP, for example |
 | Talk to a healthcare professional on your diabetes team—your consultant, diabetes specialist nurse, or diabetes specialist dietitian, for example. As a helpful way to start the conversation, you could consider completing a diabetes distress questionnaire (like the Problem Areas in Diabetes questionnaire) and taking it to your next appointment. |
 | Talk to another healthcare professional whom you trust, like your GP, for example |
What things have you found helpful through your life with diabetes to manage diabetes distress and burnout?
Read about other people’s experiences and share your own here:
Go to ‘Diabetes distress and burnout’ to return to the main topic page, or choose another section.

This module has made me feel very emotional, as have the all so far! Diabetic stress and burnout are very new terms to me and in my life when perhaps going through these I’ve not had support maybe needed to cope with this and it’s affected my life very negatively. As mentioned it’s relatively new concept so I’m sure the support will be there in the future should I need plus I have some new awareness & knowledge 😊 about it.
interesting
Never thought about burnout stress but it’s always there. You just have to get back on with it now I know it exists should make it easier
I was diagnosed at 29 now 58 this is the first time of hearing about distress and burnout. I’ve always dealt with everything myself, I’ve suffered with both many times over the years, but my daughter the one I rely on to bring me back to earth, when I want to give up on living. I know now that others have the same thoughts and problems and I will now ask for help.
Realizing others have the same difficulties has made me feel more positive that a change can be made.
I’m going to speak to my consultant at my appointment about diabetic burn out. As i went through this module i actually started crying as i have all these feeling and i realise now its not just me being stupid and not being able to cope others go through to and the doctor may understand as i have been avoiding seeing them because of it. Im starting to feel better about it now.
It can be emotional dealing with diabetes, sometimes you feel very alone through it and sometimes its hard to talk to people, mainly I am a very positive person but I do understand the concept of Diabetes burnout/distress, it definitely new as this is the first time I have heard about it in my 34 years of being type 1
Talking to health care professionals or loved ones really helps. Just someone listening validates what you are feeling